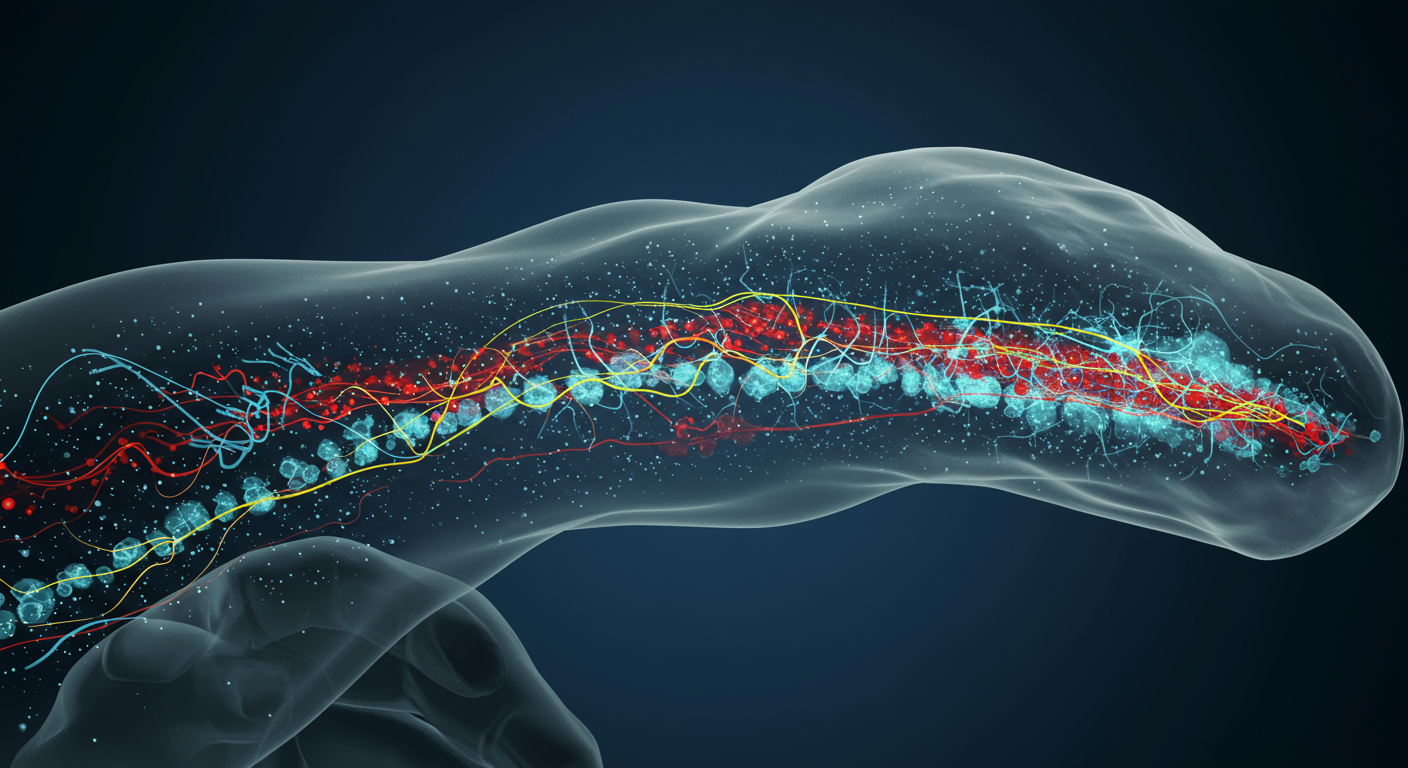
Researchers using a powerful computational approach have identified an existing drug that successfully regenerates nerve cells and improves function in animal models of spinal cord injury. A team at the University of California San Diego School of Medicine employed bioinformatics to sift through massive databases, matching the genetic signature of nerve growth to a compound called Thiorphan. The drug, previously tested in humans for other ailments, demonstrated a remarkable ability to stimulate growth in cultured adult human neurons and restore significant motor function in rats with spinal cord damage.
Spinal cord injuries often lead to permanent paralysis because neurons in the central nervous system do not naturally regenerate after damage. The search for effective treatments has been slow, but this new strategy represents a significant acceleration in the drug discovery process. By repurposing a compound with a known safety profile, the scientists have potentially cleared the first major hurdle for clinical use, paving a faster route to human trials. This data-driven method not only provides a promising candidate for spinal cord injury therapy but also establishes a new model for finding treatments for other intractable neurological disorders.
A Computational Shortcut to Drug Discovery
The foundation of the breakthrough was a unique gene pattern linked to nerve regeneration. Scientists first identified a specific signature of gene activation that occurs in mouse neurons under certain experimental conditions that encourage growth. This pattern represented a molecular fingerprint for regeneration. Instead of attempting to build a new drug from scratch, the research team turned to bioinformatics to find an existing key for this genetic lock.
Using this distinct gene expression signature, they screened a vast database of pharmaceutical compounds. The goal was to find a molecule capable of switching on this same pro-regenerative program in neurons. The data-driven analysis pinpointed Thiorphan as a top candidate, singling it out from countless other substances for its potential to mimic the cellular conditions needed for nerves to repair themselves. This method effectively serves as a high-speed matching service between a desired biological effect and a compound that can produce it.
From Database to Laboratory Bench
The identification of Thiorphan was just the first step; the team then had to validate the computational prediction in biological systems. This phase of the research produced some of the most significant findings, demonstrating that the drug’s predicted effects were reproducible in living cells.
Success in Human Cells
In a major technical achievement, the researchers applied Thiorphan to adult human brain cells cultured in the lab. These cells are notoriously difficult to grow and study, making direct tests for regenerative therapies on human neurons exceptionally rare. The experiments were a success, showing that Thiorphan significantly increased neurite outgrowth—the process of neurons extending new branches, which is a crucial metric for regeneration. This was the first time a drug candidate had demonstrated such clear effectiveness in adult human brain cells, providing strong evidence that its regenerative capacity could translate to patients.
Promising Recovery in Animal Models
Building on the cellular results, the team tested the drug in rats with spinal cord injuries. The outcomes in these preclinical models further bolstered the case for Thiorphan as a viable therapy. When administered alone, the drug led to a 50% increase in the recovery of hand function compared to untreated animals. This demonstrated that the compound could drive meaningful functional improvement on its own.
The researchers also explored a combination therapy approach. When they paired Thiorphan with a neural stem cell graft at the injury site, the results were even more pronounced. This combined treatment improved recovery by an additional 50% over the drug alone. This synergistic effect suggests that Thiorphan could become a core component of a multi-faceted strategy, enhancing the environment for nerve growth while transplanted cells help rebuild neural circuits.
The Accelerated Path to Clinical Application
One of the most promising aspects of this discovery is Thiorphan’s history. Because the drug has already undergone safety testing in humans for non-neurological conditions, the pathway to clinical trials for spinal cord injury is significantly shorter. It has cleared many of the initial safety and toxicology hurdles that new experimental drugs face, a process that can take years. This allows researchers to focus more quickly on testing its efficacy for nerve regeneration in patients.
This work fits into a broader landscape of regenerative medicine that seeks to overcome the formidable barriers to healing in the spinal cord, such as the formation of glial scars and the lack of intrinsic growth signals. While other strategies like stem cell transplantation and advanced biomaterials continue to evolve, the identification of a small-molecule drug that promotes regeneration offers a more accessible and potentially widespread therapeutic option.
A New Paradigm for Neurotrauma Research
This study is a powerful illustration of how modern technologies are converging to revolutionize medical research. The entire discovery pipeline—from gene sequencing that revealed the regeneration signature to the bioinformatics that matched it with a drug—was made possible by advances in computational power and molecular biology. According to senior author Dr. Mark H. Tuszynski, the ability to culture and test on adult human brain cells in large numbers provides a potent new platform for discovering treatments across a range of neurological disorders.
By harnessing bioinformatics to repurpose an existing drug, the UC San Diego team has created a blueprint for future research. This data-first approach can be adapted to target other diseases where cellular regeneration is the goal. It marks a shift away from traditional, slower methods of drug discovery and toward a more efficient, targeted process that could bring new hope to patients with spinal cord injuries and other conditions long considered untreatable.