A recent study has identified two distinct brain circuits originating from a single, deep brain region that independently control memory and mood, both of which are impaired by Alzheimer’s disease. The research, conducted on mouse models, demonstrated that by selectively stimulating these separate pathways, it was possible to rescue either memory function or emotional well-being, suggesting a new, more precise approach to treating the multifaceted symptoms of this neurodegenerative disorder.
The discovery moves beyond the prevailing focus on the molecular hallmarks of Alzheimer’s, such as amyloid plaques and tau tangles, to explore the specific neural highways that malfunction and give rise to the disease’s cognitive and psychological symptoms. By pinpointing that memory and mood are governed by different sets of cells within the same brain area, the findings open the door to developing therapies that can be tailored to address the full spectrum of challenges faced by patients, potentially offering a more holistic way to manage the condition. The study was led by researchers at the UNC School of Medicine and published in the journal Neuron.
Untangling Memory and Mood Circuits
The investigation centered on a small, deep brain structure called the supramammillary nucleus (SuM), located in the posterior hypothalamus. While this region has been implicated in both memory and mood regulation, the precise cellular mechanisms have remained unclear. The researchers identified two distinct populations of neurons within the SuM that project to different parts of the brain. One group of these neurons sends signals to the hippocampus, a well-known hub for memory formation and recall. The other group communicates with the medial septum, an area more closely associated with regulating emotions.
In Alzheimer’s model mice, the study revealed that both of these circuits were dysfunctional. This observation aligns with the clinical presentation of Alzheimer’s in humans, where cognitive decline is often accompanied by significant mood changes, such as anxiety and depression. The researchers hypothesized that the deterioration of these two pathways contributed independently to the different types of symptoms. This cellular-level insight provides a more nuanced understanding than broader theories focused solely on protein accumulation.
Precision Targeting Restores Brain Function
Activating Pathways with Light
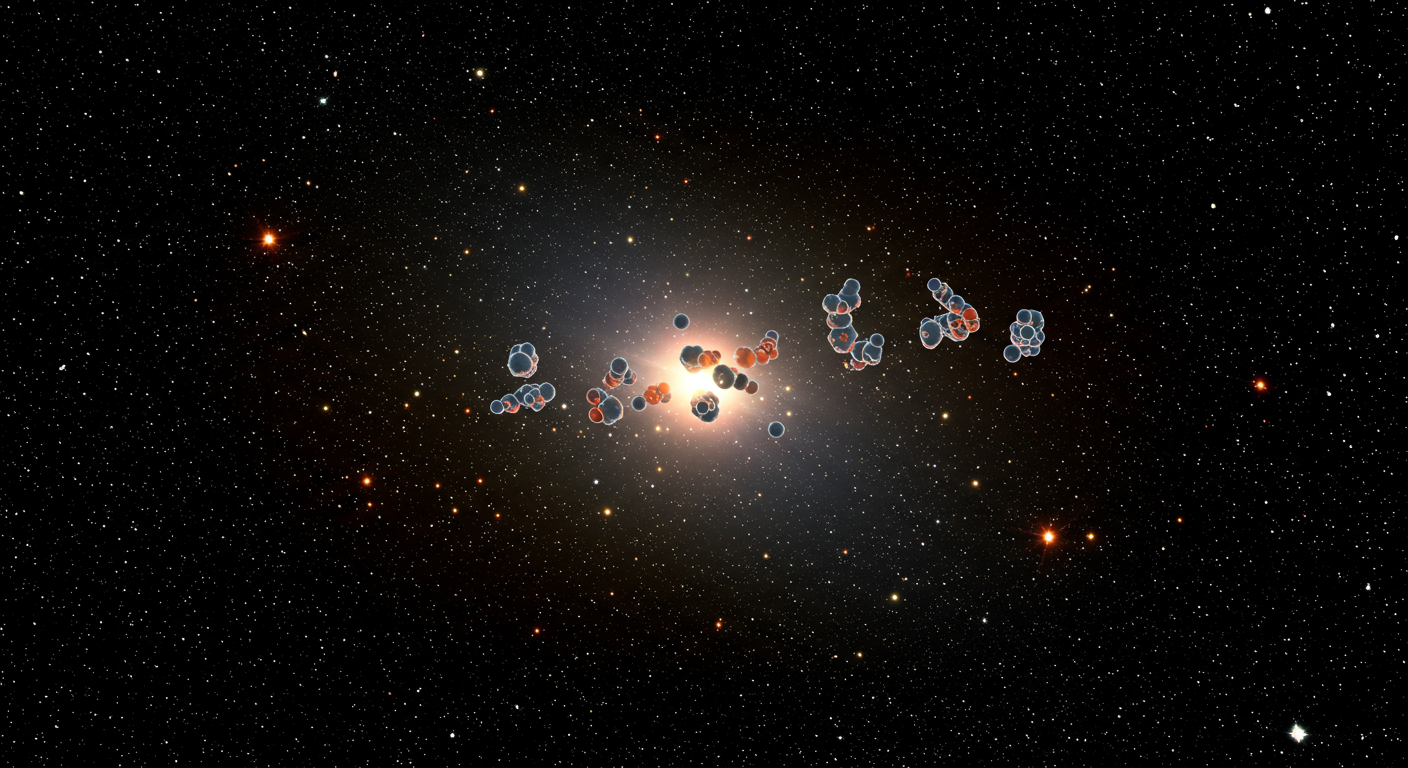
To test their hypothesis, the scientists employed a technique known as optogenetics, which uses light to control genetically modified neurons. By introducing light-sensitive proteins into the specific brain cells of the SuM, they were able to selectively activate either the memory-related circuit or the mood-related circuit in the Alzheimer’s model mice. This method allowed them to isolate the effects of each pathway with a high degree of precision.
When the pathway connecting the SuM to the hippocampus was stimulated, the mice showed significant improvements in memory tasks, performing similarly to healthy mice. Conversely, when the pathway to the medial septum was activated, the mice exhibited reduced anxiety-like behaviors, indicating a restoration of normal mood function. “We were surprised that by selectively activating each pathway, we were able to restore either memory or mood in Alzheimer’s-model mice,” stated Dr. Juan Song, the study’s senior author. “This level of precision in how a single brain region contributes to two very different symptoms—cognitive decline and anxiety or depression—was unexpected and highlights an exciting new avenue for targeted therapies.”
A New Perspective on Alzheimer’s Complexity
Current research into Alzheimer’s has predominantly focused on the accumulation of amyloid-beta plaques and tau tangles in the brain, which are thought to be the primary drivers of neuronal death and dysfunction. While these protein-centric models have been invaluable, they have yet to yield universally effective treatments. This has led some scientists to explore other contributing factors and downstream consequences, such as neuroinflammation and the specific vulnerabilities of neural circuits. The new findings add a critical layer to this understanding by demonstrating how the disease’s pathology translates into specific functional deficits at the circuit level.
Other research has also begun to map out the complex pathways to Alzheimer’s, with some studies identifying multiple trajectories involving mental health, vascular disease, and other factors that can lead to cognitive decline. The UCLA Health study, for instance, used electronic health records to trace patterns of disease progression. Similarly, work from Stanford University has explored how inflammation and amyloid-beta might converge on a single receptor to cause synapse loss. The UNC study complements this body of work by providing a tangible example of how distinct symptom domains are encoded in parallel circuits that are separately vulnerable to the disease process.
Implications for Future Alzheimer’s Therapies
Beyond a One-Size-Fits-All Approach
Most Alzheimer’s treatments in development aim to slow cognitive decline, often by targeting amyloid or tau. However, the emotional symptoms, such as anxiety, depression, and apathy, are also profoundly debilitating for patients and their families. The discovery that memory and mood circuits can be targeted separately suggests that future therapeutic strategies could be more personalized. For example, a patient experiencing severe anxiety but relatively mild memory loss could potentially receive a treatment focused on the mood-related pathway.
This circuit-based approach could lead to the development of novel interventions, including highly targeted deep brain stimulation or new classes of drugs designed to modulate the activity of specific neural pathways. “This could mean moving toward more personalized, circuit-based therapies that not only preserve memory but also improve emotional well-being, helping patients and families manage the full spectrum of challenges that come with Alzheimer’s,” Dr. Song explained. While translating these findings from mice to humans will require significant further research, this study provides a promising new framework for thinking about and treating this devastating disease.
Addressing the Full Spectrum of Symptoms
The psychological burden of Alzheimer’s is a critical aspect of the disease that can significantly impact quality of life long before the most severe cognitive impairments set in. Mood and anxiety disorders are common in people with Alzheimer’s, yet they are often viewed as secondary consequences of the cognitive struggle. This new research reframes these symptoms as a direct result of the disease’s impact on specific emotional circuits in the brain. By validating this connection, the study underscores the importance of treating the whole person, not just their memory deficits.
Understanding the distinct biological underpinnings of emotional and cognitive symptoms can also help reduce the stigma associated with the psychological aspects of dementia. It reinforces the idea that these are not simply emotional reactions to the disease but are a core part of the neurobiology of Alzheimer’s. As research continues to unravel the intricate ways in which Alzheimer’s dismantles the brain, a focus on restoring function to specific, well-defined circuits offers a beacon of hope for more effective and comprehensive treatments in the future.