A common fungus in the human mouth maintains a stealthy existence by carefully controlling the release of a potent toxin, allowing it to colonize oral surfaces without triggering a full-scale immune alarm, a new study reveals.
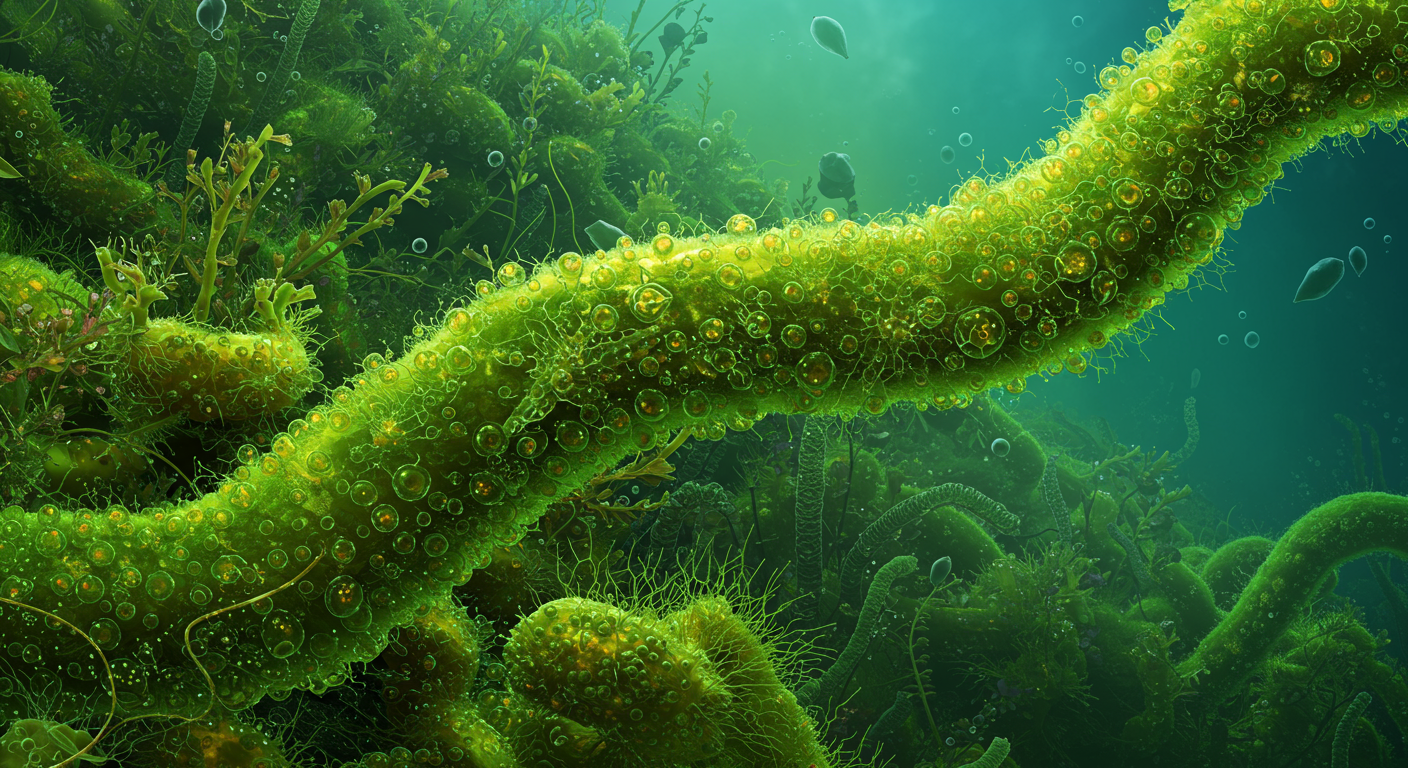
The fungus, Candida albicans, is a master of adaptation, living as a harmless member of the oral microbiome in roughly half the human population. Yet, it is also a dangerous opportunist, capable of causing debilitating oral infections (thrush) and life-threatening systemic disease in vulnerable individuals. Researchers have now uncovered a key mechanism behind this dual identity: the fungus finely tunes the production of a cell-damaging toxin called candidalysin, keeping it at levels high enough to aid colonization but low enough to avoid provoking a strong inflammatory response from host cells.
This discovery illuminates the delicate molecular negotiations that occur between a host and a resident microbe, explaining how an organism armed with pathogenic weapons can choose a strategy of quiet coexistence. The findings have significant implications for developing new therapies that could disarm the fungus rather than trying to kill it, potentially offering a way to prevent infections without driving the evolution of drug resistance.
The Toxin’s Double-Edged Sword
At the heart of the fungus’s strategy is candidalysin. This small protein, a type of peptide toxin, is a critical virulence factor for C. albicans. When the fungus grows in its invasive, hyphal form—a state where it extends long, filament-like structures—it secretes candidalysin. The toxin functions by punching holes in the membranes of host cells, particularly the epithelial cells lining the mouth. This damage serves two purposes for the fungus: it helps the hyphae penetrate tissue and it liberates nutrients, like iron, from the damaged cells.
However, candidalysin is also a powerful beacon for the human immune system. Oral epithelial cells are not passive bystanders; they are frontline sentinels. When they detect the damage caused by candidalysin, they initiate a powerful pro-inflammatory cascade. This response, mediated by a cellular machinery component known as the NLRP3 inflammasome, releases signaling molecules called cytokines that recruit neutrophils and other immune cells to the site of infection to clear the fungus. A strong response leads to the inflammation, pain, and white lesions characteristic of oral thrush.
This presented a paradox for scientists: if candidalysin is so effective at triggering immunity, how does C. albicans manage to live peacefully in the mouths of millions of healthy people without constantly causing inflammation? The new research suggests the answer lies not in whether the toxin is produced, but in how much.
A Finely Tuned Balance
To investigate this balance, scientists utilized advanced models of the human oral mucosa, including three-dimensional organoid cultures grown from human epithelial cells. These models provide a much more realistic environment for studying host-pathogen interactions than traditional flat cell cultures. Researchers exposed these oral tissues to different strains of C. albicans.
The experimental approach likely involved comparing several fungal strains:
- A standard, or “wild-type,” C. albicans strain capable of normal toxin production.
- A mutant strain engineered to be incapable of producing candidalysin.
- A second mutant strain engineered to overproduce the toxin, releasing it at constitutively high levels.
By monitoring the host tissues, the research team found that the wild-type fungus caused only minimal, low-level damage and triggered a correspondingly mild immune response. In contrast, the candidalysin-overproducing strain provoked a massive inflammatory reaction, while the strain lacking the toxin altogether was less effective at colonizing the tissue. This demonstrates that a “Goldilocks” level of toxin production—not too much, not too little—is optimal for the fungus to establish a stable, long-term residence.
The fungus achieves this control by tightly regulating the gene that codes for candidalysin, known as ECE1. During the commensal, or harmless, state, the fungus keeps expression of this gene at a low baseline. This produces just enough toxin to facilitate adherence and nutrient acquisition without crossing the threshold that trips the host’s main inflammatory alarms.
The Switch from Friend to Foe
This tightly regulated system also explains how C. albicans can so rapidly switch from a quiet commensal to an aggressive pathogen. The transition is not caused by the fungus acquiring new weapons, but by a change in the environment that gives it the green light to deploy its existing arsenal at full force.
Several factors can disrupt the delicate oral ecosystem and trigger this switch. A course of broad-spectrum antibiotics, for example, can wipe out the resident bacteria that normally compete with C. albicans and keep its growth in check. With its competition gone, the fungus can proliferate and ramp up ECE1 expression and candidalysin secretion, overwhelming the host’s defenses.
Most critically, the host’s immune status is a key determinant. In individuals with compromised immune systems—such as those with HIV/AIDS, cancer patients undergoing chemotherapy, or organ transplant recipients on immunosuppressive drugs—the immune surveillance that normally contains the fungus is weakened. Sensing this vulnerability, C. albicans can increase its toxin production, leading to invasive disease that can spread from the mouth into the bloodstream, a condition known as systemic candidiasis, which carries a mortality rate of over 40%.
Implications for Future Therapies
Understanding this regulatory balancing act opens a new front in the battle against fungal infections. Traditional antifungal drugs work by killing the fungus, but their widespread use has led to a concerning rise in drug-resistant strains. The new findings point toward an alternative “anti-virulence” strategy.
Instead of seeking to eradicate the fungus, future therapies could target the specific regulatory pathways that control candidalysin production. A drug that prevents C. albicans from upregulating the ECE1 gene would effectively disarm it, leaving it unable to cause significant tissue damage. This would allow even a weakened immune system to manage the fungal population, preventing the transition from harmless colonization to active infection.
Researchers are now focused on identifying the specific molecular switches and environmental cues that C. albicans uses to modulate its toxin levels. Unraveling this complex signaling network could provide multiple targets for novel drugs. Further studies in animal models will be necessary to validate this approach and determine if keeping the fungus in a commensal-like state is a viable long-term strategy for preventing disease in at-risk patient populations.